Irritable Bowel Syndrome (IBS) is a common gastrointestinal disorder characterized by recurring abdominal pain,
bloating, and changes in bowel habits. It affects millions of people worldwide and can significantly impact
their quality of life. While there is no cure for IBS, there are various management strategies that can help
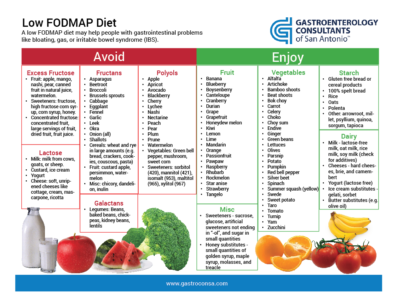
alleviate symptoms. One such approach is the FODMAP diet, which has gained popularity in recent years for its
effectiveness in reducing IBS symptoms.
What are FODMAPs?
FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) are a group of
short-chain carbohydrates and sugar alcohols that are poorly absorbed by the small intestine. Instead, they
travel to the large intestine, where they are fermented by gut bacteria, leading to gas and other
gastrointestinal symptoms in individuals with IBS.
How does the FODMAP diet work?
The FODMAP diet is an elimination diet that involves temporarily removing high-FODMAP foods from the diet and
then gradually reintroducing them to identify specific triggers. The diet is typically divided into three
phases: restriction, reintroduction, and personalization.
The Restriction Phase
During the restriction phase, individuals are instructed to avoid high-FODMAP foods for a specific period,
typically around 6-8 weeks. This includes foods containing lactose, fructose, fructans, galactans, and polyols.
High-FODMAP foods include certain fruits, vegetables, dairy products, legumes, wheat, and sweeteners like
honey and agave syrup. This phase aims to reduce symptoms and allow the gut to heal.
The Reintroduction Phase
After the restriction phase, gradually reintroducing specific high-FODMAP foods helps identify individual
triggers. Foods are reintroduced in a structured manner while carefully monitoring symptoms. This phase helps
determine which FODMAPs trigger symptoms in each person, as triggers can vary between individuals. It is
crucial to keep a food and symptom diary during this phase to track responses accurately.
The Personalization Phase
Once trigger foods are identified, the personalization phase involves tailoring the diet to an individual’s
specific tolerances. This phase allows a more flexible approach, as not all high-FODMAP foods need to be
completely eliminated. Based on personal tolerances, individuals can continue to enjoy some high-FODMAP foods
without exacerbating symptoms.
Benefits of the FODMAP Diet
Numerous studies have shown that the FODMAP diet can effectively reduce IBS symptoms in up to 70% of people
with the condition. By identifying and avoiding individual trigger foods, individuals can experience reduced
bloating, abdominal pain, gas, and changes in bowel habits. The diet can significantly improve quality of life
and provide relief from the often-debilitating symptoms of IBS.
Considerations and Potential Challenges
While the FODMAP diet can be highly beneficial for IBS sufferers, it is important to consult a healthcare
professional or a registered dietitian before starting. They can guide you through the process and help ensure
nutritional adequacy during the restriction phase. Additionally, it is crucial not to continue the strict
restriction phase longer than necessary to avoid unnecessary dietary limitations.
Conclusion
The FODMAP diet is a valuable tool for managing IBS symptoms. By eliminating and gradually reintroducing
specific foods, individuals can identify their trigger foods and customize their diet accordingly, providing
relief from pain, bloating, and other gastrointestinal discomforts. However, it is essential to involve a
healthcare professional throughout the process to ensure proper guidance and a nutritionally balanced diet.
With the appropriate support, the FODMAP diet can significantly improve the quality of life for those living
with IBS.
Published on January 1, 2022